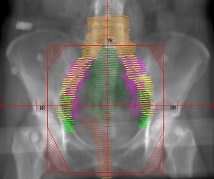
Example of a pelvic field for external beam radiation therapy (EBRT) after hysterectomy for stage I-II endometrial cancer.
This treatment uses a low radiation dose and takes place over five to six weeks, five days a week. Surrounding structures, such as the bowel and bladder, also receive some radiation, which can result in gastrointestinal and urinary side effects and tiredness. This treatment is sometimes performed preoperatively, for example if invasion of the cervix is suspected.
High-dose-rate (HDR) radiation “tampon” cylinder placed in vagina for application of internal brachytherapy (“near therapy”) after hysterectomy for endometrial cancer. The cylinder is attached to a machine by a catheter, through which radiation is delivered to the vaginal cuff incision area to prevent any microscopic cancer cells from causing a crecurrence. This therapy can also be used to shrink tumors. Each of the three to five treatments takes only minutes because of the high dose rate compared with the two to three days required for traditional low-dose-rate (LDR) vaginal therapy. This form of treatment is localized to the area of concern and delivers less radiation to surrounding structures than external radiation, resulting in fewer side effects to the bowel and bladder; however, it does narrow and dry out vaginal mucosa. Once the application cylinder is removed, the patient is not radioactive (!).
Health Update—Orange Pee
This past Tuesday, January 7, I had two appointments at St. Barnabas. First, I saw my gynecologic oncologist because of the lymphatic drainage, which seemed to abate while I was recovering from the Mohs excision of the basal cell carcinoma on my scalp, practically immobilized for a few days because of the pain. As I became more active, so did the drainage—but it wasn’t as bad as it had been originally. He did a pelvic exam and said I was healing well.
To make sure I didn’t have a fistula between the bladder and vagina, he prescribed phenazopyridine (Pyridium), pills that turn urine orange (and are also used to soothe the urinary tract for patients with an infection), and gave me a few tampons to do a test: if the top of the tampons remained clear and did not turn orange, that would mean I had no fistula (that is, no passageway that would enable urine to leak from my bladder into my vagina). Neither he nor I really thought I had a fistula because I’ve never smelled urine in the discharge. (For this reason, I declined to let him inject methylene blue dye into my bladder to check for other fistulas. If he had done both, it would have been called a “double dye test.”) The surgeon said he has only one or two patients a year who have this lymphatic drainage problem and can’t explain why. (I hope you other hysteroladies from 2013 appreciate my sacrifice. 🙂 )
Anyway, for the past few days I’ve been an orange pee-er. None of the tampons were colored orange at the top, although they were at the bottom because they were close to the urethra. All I noted at the top of the tampons was a little dark-pink blood. And the best news is that the discharge has slowed down considerably since my visit on Tuesday.
Also during the visit, the surgeon said that the radiation oncologist had called him that morning to discuss my case before she saw me for my consultation that afternoon. They discussed possible courses of radiation therapy, one being combination pelvic (external) and vaginal (internal) therapy—this alarmed me because previously the surgeon had said I would need only internal radiation. (He also said he told the radiation oncologist to be prepared for a lot of questions from this particular patient!)
Treatment Plan–Radioactive Tampons
Next, I went across the street to St. Barnabas to meet with the radiation specialist. She’s quite young and could be my daughter—I am getting used to this phenomenon of “child doctors,” but sometimes it still startles me because part of me still believes I’m their age! Her parents are from India, and this helped establish a rapport with Farok. And she was very knowledgeable and forthcoming, which helped establish a rapport with me.
She spent quite a lot of time reviewing my records and giving us an overview of how patients with endometrial cancer have historically been treated, and she also reviewed the outcomes of a few clinical studies. However, my situation falls outside the range of most patients in these studies because of the features of my endometrial adenocarcinoma: (1) stage 1B-C, meaning the tumor, which had almost completely filled my uterus, had invaded the myometrium (uterine muscle layer) almost 70% and (2) grade 3, meaning the composition of the tumor was mostly abnormal cells (the radiation oncologist actually used the word “bizarre”). These features indicate that I had an aggressive cancer, even though no visible tumor remained after surgery; combined with my age (61), this means that I am a high-intermediate risk patient for recurrence from invisible (microscopic) cells. Although this sounds pretty unsettling, the numbers aren’t really that big: with no radiation at all, the risk of recurrence would be about 15% or a bit higher because of my cancer features; with either pelvic (external) or vaginal (internal) radiation alone, the risk would be reduced by about half to 7-8%.
If I were to have combination radiation treatment, I would start with external beam radiation therapy (EBRT) five days a week for five weeks, for a total of 25 low-dose-rate (LDR) treatments to my pelvis; this would be followed by internal vaginal brachytherapy (“near therapy”) of only about four to five high-dose-rate (HDR) treatments to my vaginal cuff area. Both forms of treatment create side effects in surrounding structures, particularly the bowel, bladder, and, of course, the vagina. As it is, I have both GI and urinary issues, and being postmenopausal means I already have vaginal issues as well.
Long story short: given the dearth of abundant hard data on patients with my exact features, a pathology report that showed that the tumor had been contained within the uterus with no metastasis to surrounding organs or lymph nodes, and the potential for increased side effects with combination therapy, we decided to do just internal rather than external-internal radiation therapy. This was my choice, and the doctor agreed with it. It seems to me that so much radiation would be overkill and that the risks of side effects would outweigh the potential benefit of double treatment. Other studies have included chemotherapy, something I’m very glad not to have to experiment with. Note: As with any cancer patient, there is a small risk that microscopic cancer cells could migrate to other parts of my body, creating tumors there (for example, in the lung); such tumors, in my case, would still be considered endometrial cancer. This is an unlikely scenario.
So, I will have three “fractions” of vaginal brachytherapy, meaning I will get one-third the total radiation dose targeted to the vaginal cuff area on each of three visits scheduled about 10 days apart. Each radiation treatment should take only a few minutes. Sorry to disappoint you SF (sci-fi) fans, but after they remove the application cylinder (see diagram), I will not be radioactive and will therefore not glow in the dark.
The first visit is scheduled for January 23 to give my incision area a chance to heal further. Farok will be leaving for India just before I start treatment, so I’ll be on my own. I am in the process of finding help with transportation to get me to the radiation appointments, especially the first one. During the initial visit, they do a CAT scan to determine placement of the applicator for therapy (see diagram), which requires that I arrive with a full bladder. Then they do the first treatment, after which I may have some nausea because the small bowel descends into the area formerly occupied by the uterus and therefore receives some radiation. Although this first visit is a big time commitment–I’ll be there for several hours, and the drive is an hour each way–any help would be most appreciated.
* * *
All things considered, I am doing pretty well. I still have the stitches in my head following the scalp excision and look a little like the Bride of Frankenstein, but thankfully the pain decreased significantly after the first four days. The sutures come out on Monday, after which I will have an almost-full bottle of baby shampoo as a token of this “hair-raising” experience.
Hope everyone’s new year is getting off to a good start, despite the wacky weather.




I know it seems like it will never end, but the end is in site. Hang in there, sounds like you are the
Ibest patient advocate , for you, which means you are in good hands. Wish I could do more for you. Keeping you in my prayers. Love you. Always Linda
LikeLike
Thanks, Lin. Appreciate the kind words. Love, P
LikeLike
You can add me to the list of available drivers. I don’t have anything terribly important on the horizon but I do like to plan ahead.
I missed the book group this week because Bill has pneumonia. He’s s-l-o-w-l-y improving. I sick male is a __________(fill in the blank).
Susan
_____
LikeLike
Susan, how nice–especially because the list is getting shorter and shorter. In case it comes down to you and me, tell me whether it makes sense for me to drive to your place and you drive from there? I think it does.
I was wondering why I didn’t see you yesterday. As it turned out, all the talk was about Chris Christie and our various health issues. The only real comments about the book were that people couldn’t really connect with the characters, even though they liked the historical context.
Hope your sick male becomes an unsick one very soon–I’m sure you need a break!
Stay well, and thanks again. I’ll let you know.
Pam
LikeLike
P.S. Susan, glad we caught up by email. Really appreciate your help. Will be back in touch very soon.
LikeLike
Well I must say you are handling all this extremely well. I sincerely am grateful that you will, hopefully, have the transportation you need and the wacky weather will not return any time soon.I know it will be lonely without a husband there but I am here to talk whenever you feel the need. Sorry I don’t drive or that you are not closer. You will be constantly in my thoughts and prayers every day. Ask Farok to not stay as long as usual as you will need help. You have done a wonderful job with this blog and I am so proud of you. I love you, Mom
LikeLike
Yes, I think I have found some transportation support, which I may need if I have a reaction to the radiation. And the first day, of course, will be the toughest and longest.
Thanks for the comments about the blog–I’m glad you’ve been getting something out of it. (It takes quite a long time to write these posts!)
Love,
Pam
LikeLike
Pam,
It is an education reading your blog. I admire your ability to synthesize and process all the information while going through the tests and surgeries. To put all this information in factual form – to write it down – enables you to look back and remember clearly – everything in chronological order as it occurred. For me, I would think the recording of everything would help to reduce fear and emotion. The clarity of your writing and thinking is amazing and I continue to admire your strength and reality based approach during a very stressful time. Starting the blog was an excellent idea. Thank you. Every good wish for your health and time in 2014 to relax and feel better.
LikeLike
Thank you, Pat, for your ongoing encouragement and support.
The blog has helped me chronicle this journey–and has also kept my mind occupied and sharp, which is itself good medicine.
Hope to see you one of these days soon and that everything is going well for you so far in the new year.
Best wishes . . .
LikeLike
[…] My Current Story, Update: Uterine (Endometrial) Cancer – Orange Pee & Radioactive Tampons […]
LikeLike